 The discovery, published in the journal PLOS Biology, offers new opportunities in the treatment of cardiovascular diseases, cancer and many other diseases.
The discovery, published in the journal PLOS Biology, offers new opportunities in the treatment of cardiovascular diseases, cancer and many other diseases.
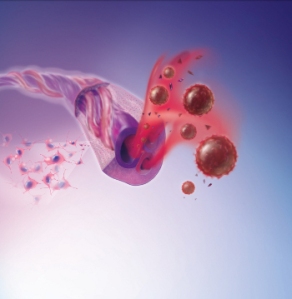
The growth of new blood vessels – angiogenesis – occurs during the repair of damaged tissue and organs in adults. However, malignant tumors also grow new blood vessels in order to receive oxygen and nutrients. As such, angiogenesis is both beneficial and detrimental to health, depending on the context, requiring therapeutic approaches that can either help to stimulate or prevent it. Therapeutics that aim to prevent the growth of new blood vessels are already in use, but the results are often more modest than predicted.
For more than a decade, Prof Petri Salvén of the University of Helsinki and his colleagues have studied the mechanisms of angiogenesis to discover how blood vessel growth could be prevented or accelerated effectively.
“We succeeded in isolating endothelial cells with a high rate of division in the blood vessel walls of mice. We found these same cells in human blood vessels and blood vessels growing in malignant tumors in humans. These cells are known as vascular endothelial stem cells. In a cell culture, one such cell is capable of producing tens of millions of new blood vessel wall cells,” Prof Salvén said.
From their studies in mice, the team was able to show that the growth of new blood vessels weakens, and the growth of malignant tumors slows, if the amount of these cells is below normal. Conversely, new blood vessels form where these stem cells are implanted.
“The identification and isolation of an entirely new adult stem cell type is a significant discovery in stem cell biology. Endothelial stem cells in blood vessels are particularly interesting, because they offer great potential for applications in practical medicine and the treatment of patients,” Prof Salvén said.
“If an efficient method of vascular endothelial stem cell production could be developed, it could offer new treatment opportunities in situations where damaged tissue or diseases call for new blood vessel growth, or where the constriction or dysfunction of blood vessels deprives tissues of oxygen, for example in cardiac disease. These cells also offer new opportunities for developing therapeutics that seek to prevent new blood vessel growth in malignant tumors.”


You must be logged in to post a comment.