 Japanese scientists have used induced stem cells to create a liver-like tissue in a dish.
Japanese scientists have used induced stem cells to create a liver-like tissue in a dish.
Although they have yet to publish their results and much work remains to be done, the achievement could have big clinical implications. If the results bear out, they would also constitute a significant advance in the ability to coax stem cells to self-organize into organs.
The work was presented by Takanori Takebe, a stem-cell biologist at Yokohama City University in Japan, at the annual meeting of the International Society for Stem Cell Research in Yokohama last week. “It blew my mind,” said George Daley, director of the stem-cell transplantation programme at the Boston Children’s Hospital in Massachusetts, who chaired the session.
“It sounds like a genuine advance,” says Stuart Forbes, who studies liver regeneration at the University of Edinburgh, UK. Forbes, who also works as a consultant for Scotland’s liver-transplantation unit, says that the advance could one day help to avoid the “bleak outcome” currently experienced by the many patients who don’t survive long enough to get a new liver.
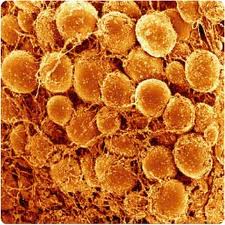
But the liver described by Takebe has a long way to go before that. Takebe told how his team grew the organ using induced pluripotent stem cells (iPS), created by reprogramming human skin cells to an embryo-like state. The researchers placed the cells on growth plates in a specially designed medium; after nine days, analysis showed that they contained a biochemical marker of maturing liver cells, called hepatocytes.
At that key point, Takebe added two more types of cell known to help to recreate organ-like function in animals: endothelial cells, which line blood vessels, taken from an umbilical cord; and mesenchymal cells, which can differentiate into bone, cartilage or fat, taken from bone marrow. Two days later, the cells assembled into a 5-millimetre-long, three-dimensional tissue that the researchers labelled a liver bud — an early stage of liver development. 
The tissue lacks bile ducts, and the hepatocytes do not form neat plates as they do in a real liver. In that sense, while it does to some degree recapitulate embryonic growth, it does not match the process as faithfully as the optic cup recently reported by another Japanese researcher. But the tissue does have blood vessels that proved functional when it was transplanted under the skin of a mouse. Genetic tests show that the tissue expresses many of the genes expressed in real liver. And, when transferred to the mouse, the tissue was able to metabolize some drugs that human livers metabolize but mouse livers normally cannot. The team claims that its work is “the first report demonstrating the creation of a human functional organ with vascular networks from pluripotent stem cells”.
Takebe says the success depended on properly timing the addition of the other two cell types. “It took over a year and hundreds of trials,” says Takebe.
The team says that the tissue’s three dimensions will give it advantages over simple cell-replacement therapies. It could be used for long-term replacement or short-term graft while the recipient waits for a suitable liver donor, or in cases in which doctors anticipate that the native liver will eventually regain its function. But such applications would require extensive development, including making sure that the tissue contains the proper arrangement of lobules.
It won’t be easy, says Forbes. To treat the commonest reason for liver transplants, chronic liver disease, the cells would have to be stable, potentially for many years, in the patient. But it is not clear whether that would be possible, especially considering that they would be exposed to many toxins and pathogens. Furthermore, the organ would need to stay the right size, without atrophying or developing cancerous growth. “Any deviation from the mature phenotype could be catastrophic for the graft,” says Forbes.
Other researchers have developed competing technologies using scaffolds to build three-dimensional liver-like structures. Sangeeta Bhatia, a bioengineer at the Massachusetts Institute of Technology in Cambridge, for example, has produced a scaffold-based graft that doesn’t try to recapitulate development but has proved to be functional and transplantable in mice. Bhatia is now working on increasing the number of hepatocytes present on the two-centimetre graft, to ensure that it is useful in the clinic. “One billion cells is the next frontier,” she says.
In the meantime, Takebe and the rest of the team, led by Hideki Taniguchi, also a stem-cell biologist at Yokohama City University — who are collaborating on the project with researchers at Sekisui Medical, a biotechnology firm based in Tokyo — hope that his liver bud could be useful for toxicity testing in drug screening, for which bile ducts are not needed. Many conventional hepatocyte cells that are transplanted to mice for in vivo testing last for only two or three days, but the drug and its various metabolites might take weeks to metabolize, so toxic effects might not be apparent in such testing. Takebe says his graft has the necessary staying power.
Many researchers are already growing hepatocyte-like cells: Bhatia, for example, has already commercialized a device that uses bioengineered cells for drug testing. However, Takebe’s liver bud has the advantage of being grown from iPS cells, rather than, for example, the primary human hepatocytes used in Bhatia’s graft, which could make it useful in modelling rare diseases or examining the specific genetic backgrounds of the iPS cell donors.
Markus Grompe, who studies liver disease at the Oregon Health and Science University in Portland, says that Takebe’s team is “on the right track”. Still, he says, the liver cells need to function much more efficiently than they do at present. On the basis of a cursory inspection of Takebe’s data presented at the meeting, Grompe says that the liver bud was producing only a small fraction of the albumin — a plasma protein that is a key marker of liver function — that it should. But Takebe says that since his group generated the data presented at the Yokohama meeting, procedural improvements have already led to higher levels of albumin.
The next step for the team is to try to make the liver bud more liver-like, by including structures such as bile ducts.
Source: David Cyranoski, Nature




You must be logged in to post a comment.